The coronavirus (COVID-19) pandemic has proven to be a formidable scientific, medical, and social challenge. The complexity of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is centered on the unpredictable clinical course of the disease that can rapidly develop, causing severe and deadly complications.
Overview of the COVID-19 biomarker landscape
Below is the list of biomarkers which play a pivotal role in disease pathogenesis and its levels change according to the severity of COVID-19 infection. The identification of effective laboratory biomarkers able to classify patients based on their risk is imperative in being able to guarantee prompt treatment.
Inflammatory markers:
In SARS-CoV-2 infected patients, retrospective analysis has demonstrated that initial plasma levels of IL-1beta, IL-1RA, IL-7, IL-8, IL-10, IFN-gamma, monocyte chemoattractant peptide (MCP)-1, macrophage inflammatory protein (MIP)-1A, MIP-1B, granulocyte-colony stimulating factor (G-CSF), and tumor necrosis factor-alpha (TNF-alpha) were ‘increased in patients with COVID-19’. Further analysis has shown that the plasma concentrations of IL-2, IL-7, IL-17, IL-10, MCP-1, MIP-1A, and TNF-alpha in ICU patients were ‘higher than non-ICU patients’. Moreover, the plasma levels of IL-2, IL-6, IL-8, IL-10, and TNF-alpha, observed in severe infection, were prominently greater than those in non-severe infection.
Studies have revealed that levels of IL-6, the most common type of cytokine released by activated macrophages, rise sharply in severe manifestations of COVID-19. However, since most studies to date have been observational, it is difficult to extrapolate if the rise is significant enough to cause the manifestations seen in severe forms.
CRP a plasma protein produced by the liver and induced by various inflammatory mediators such as IL-6. Despite being non-specific, this acute phase reactant is used clinically as a biomarker for various inflammatory conditions; a rise in CRP levels are associated with an increase in disease severity. As per Wang et al. 2020 in retrospective cohort; greater CRP values correspond with the critical group, as groups were determined based on the diameter of largest lung lesion – CRP levels may indicate lung damage and development of disease.
Lactate dehydrogenase has been described to be increased during acute and severe lung damage, and elevated LDH values has been found in other interstitial lung infections. In COVID-19 patients LDH and CRP might represent an expression of lung damage and might reflect the respiratory distress consequent to the abnormal inflammation status.
Chemokine (C-X-C MOTIF) Ligand:
Studies by Kyung et al. have shown that, C-C motif (CC) chemokines (CC chemokine ligand [CCL] 2, CCL7, CCL8, CCL24, CCL20, CCL13, and CCL3), C-X-C motif (CXC) chemokines (CXC chemokine ligand [CXCL] 2 and CXCL10), and chemokine receptor subfamilies were most numerous, and were significantly (FDR < 0.05) upregulated in both mild and severe COVID-19 patient groups.
Hematologic biomarkers:
These used to stratify COVID-19 patients include WBC count, lymphocyte count, neutrophil count, neutrophil–lymphocyte ratio (NLR), platelet count, eosinophil count, and hemoglobin. Studies by Yang et al. reported lymphopenia in 80% of critically ill adult COVID-19 patients. These observations suggest that lymphopenia may correlate with infection severity. Qin et al. analyzed markers related to dysregulation of immune response in a cohort of 450 COVID-19 positive patients, reporting that severe cases tended to have lower lymphocyte-, higher leukocyte-counts and higher NLR, as well as lower percentages of monocytes, eosinophils, and basophils compared to mild cases.
Studies have revealed that although there were evident differences in lymphocytes (lymphocytopenia), platelet count and D-dimer in patients who experienced composite endpoints (ICU admission, invasive mechanical ventilation and death) there was no statistical analysis performed. In another study lowest platelet count associated with mortality. Moreover, both CD4+T and CD8+T counts significantly reduced in severe COVID-19 group compared with non-severe group.
D-dimer:
D-dimer originate from the lysis of cross-linked fibrin with rising levels indicating the activation of coagulation and fibrinolysis. Studies have associated COVID-19 with hemostatic abnormalities with one study observing elevated levels of D-dimer, the measure of coagulation, in non-survivors compared to survivors and its levels rose throughout until death.
Ferritin:
Elevated serum ferritin is a useful marker for a possible disease progression towards a critical development of COVID-19, it remains unclear whether serum ferritin concentration reliably reflects disease severity and whether serum ferritin can be used to gauge therapeutic effects.
ACE2:
ACE2 protein at the surface of lung alveolar epithelial cells allows infection of the respiratory tract with SARS-CoV-2. It can be hypothesized that the ACE2 levels correlate with susceptibility to SARS-CoV-2 infection. Apparently, men have a higher ACE2 expression in lung than women and Asian people express ACE2 higher than Caucasian and African American populations. This is in agreement with findings that conversion of Ang II to Ang by ACE2 was higher in males than female, suggesting an over-expression of ACE2 in men.
Procalcitonin:
Studies by Rui Hi, have demonstrated that procalcitonin may be an indicator of disease severity and may contribute to determining the severity of patients with COVID-19.
Immunoglobulins:
Most emerging studies described serological tests based on detection of SARS-CoV-2-specific IgM and IgG.1–4. Although detection of SARS-CoV-2-specific IgA in serum has been reported in few papers, analyses of IgA levels in a larger number of COVID-19 patients are still lacking.
Studies by Huan et al have demonstrated that serum IgM and IgG levels in moderate and severe COVID-19 patients were significantly higher than mild cases, while no significant difference was observed between severe and moderate patients. However, we found that IgA levels in severe cases were significantly higher than those mild or moderate cases.
COVID-19 biomarker findings in GOBIOM database
The diagnostic biomarkers for COVID-19 in GOBIOM database are in-line with the findings in the literature. Below are the top diagnostic biomarkers for COVID-19 diagnosis from GOBIOM database:
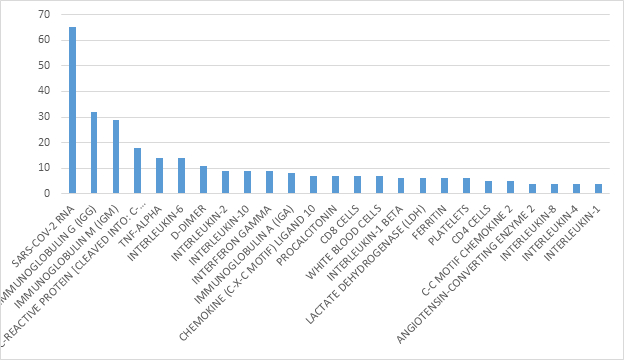
Figure1: Top Biomarkers in COVID-19 diagnosis from GOBIOM database
Utility of Excelra's GOBIOM in COVID-19 research
We highlight the important biomarkers involved in COVID-19 diagnosis along with how the levels of biomarkers may change according to severity of COVID-19 infection. This can be used as an adjunct in clinical practice to guide treatment and admission to ICU. By doing so, it may improve prognosis and minimize the mortality rates.
In this manner, focused biomarker databases like GOBIOM can be a very useful resource to identify biomarkers predictive of drug response or resistance, further facilitating selection of right patient population who are most likely to respond to treatment.


