Contributors : Chandra Sekhar Pedamallu
Date : Mar’25
Introduction
Cancer treatment is gradually evolving from the classical use of non-specific cytotoxic drugs targeting generic mechanisms of cell growth and proliferation. Today, insights from research have enabled the development of personalized treatment tailored to patients’ tumor-specific molecular markers. This includes druggable genomic alterations such as oncogenic driver mutations, which could lead to targeted cancer therapy. Treatments based on predictive biomarkers form the foundation of precision oncology, which aims to deliver targeted therapy to patients and is an evolving landscape for personalized medicine. The long-term vision for precision medicine is to identify an optimal therapy for the patient that will maximize their survival and quality of life while minimizing off-target side effects.
In this blog, we will talk about urothelial carcinoma, also known as transitional cell carcinoma, and how some recent research and discoveries help develop precision medicines and improve patient’s quality of life. Urothelial carcinoma is a type of cancer that typically starts in the urothelial cells lining the urinary tract, including the bladder, ureters, and renal pelvis. It is the most common type of bladder cancer. Symptoms may include blood in the urine, frequent urination, and pain during urination. Treatment options depend on the stage and location of the cancer and can include surgery, chemotherapy, radiation therapy, and immunotherapy. Early detection and treatment are essential for better outcomes. This has become a critical health issue worldwide, with over 614,298 new cases diagnosed annually and over 200,000 deaths due to it as reported by World Cancer Research Fund in 2022. Data from the National Cancer Institute (Surveillance, Epidemiology, and End Results Program) suggests an estimated 83,190 new cases of bladder cancer (4.2% of all cancer cases) and 16 840 estimated deaths (2.8% of all cancer deaths) in 2024 in the US, with 5-year survival rate (78.4%). However, Asian populations stand out due to unique genetic patterns. This provides valuable insights into the disease’s biology and opens avenues for innovative therapeutic strategies.
A recent systematic review delves into the prevalence and clinical implications of Fibroblast Growth Factor Receptor 3 (FGFR3) genomic alterations in Asian bladder cancer patients, shedding light on a promising frontier in precision oncology.
FGFR3: One of the Key Oncogenic Drivers
FGFR3 is a key gene in bladder urothelial carcinoma, frequently exhibiting mutations and structural variants contributing to tumor growth. Among Asian patients, FGFR3 alterations, including the hotspot S249C mutation, occur in up to 18.4% of cases, making it a common alteration in this demographic. These mutations are often mutually exclusive with TP53 alterations, suggesting distinct oncogenic pathways. This underscores FGFR3’s role as a critical driver in certain bladder cancer patients, providing a targeted opportunity for therapeutic intervention.
| SI.No. | Country | New Cases |
|---|---|---|
| 1 | US | 80404 |
| 2 | China | 92883 |
| 3 | Italy | 34580 |
| 4 | Japan | 34568 |
| 5 | Germany | 29035 |
| 6 | UK | 23643 |
| 7 | India | 22548 |
| 8 | Spain | 21418 |
| 9 | France (Metropolitan) | 19733 |
| 10 | Russia | 19352 |
| Total (Global) | 614298 | |
Table.1 Global bladder urothelial carcinoma incidence (2022)
Statistics from: Bladder cancer statistics | World Cancer Research Fund
Targeted Therapeutic Intervention Focussing on FGFR3, the Key Oncogenic Driver
FGFR3 has emerged as a pivotal gene in bladder urothelial carcinoma, frequently showing mutations and structural variants that drive tumor growth. Tumor protein p53 (TP53) is a gene that codes for a tumor suppressor protein, cellular tumor antigen p53. The protein regulates gene expression in cell cycle arrest, apoptosis, senescence, DNA repair, and changes in metabolism (Gene 2014). In cancer, TP53’s normal roles are not fulfilled, leading to cell survival, DNA damage, and cell proliferation. TP53 is the most frequently mutated gene in cancer; it is mutated in about half of all cancers (Genetics Home Reference 2014).
Since FGFR3 mutations are often mutually exclusive with TP53 alterations, the exclusivity highlights FGFR3’s role as a critical driver in certain bladder cancer subtypes, offering a focused target for therapeutic intervention.
Clinical Implications of FGFR3 Alterations
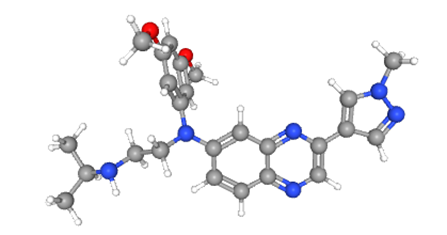
FGFR3 gene plays a crucial role in various biological processes, such as skeletal development. Mutations in this gene can lead to a range of human diseases related to skeletal dysplasias and even certain types of cancers. Understanding the functions and mutations of the FGFR3 gene is important for developing targeted therapies and improving patient outcomes. A notable breakthrough came when Erdafitinib (Balversa, Janssen Pharmaceuticals) the first small-molecule FGFR inhibitor (Figure 2) got approval from FDA for use in advanced bladder cancer harboring FGFR3 or FGFR2 genetic alterations.
Figure.2 : Erdafitinib (From PubChem Erdafitinib | C25H30N6O2 | CID 67462786 – PubChem)
Clinical trials of Erdafitinib have demonstrated promising results, with an overall response rate exceeding 30% and manageable side effects. These results provide hope for improved interventions and patient outcomes.
Precision Medicine: Guiding Better Outcomes
Molecular profiling is key in bladder cancer management. Identifying FGFR3 mutations and structural variants not only guides targeted therapies but also helps in understanding tumor biology.
The mutual exclusivity of FGFR3 and TP53 mutations further suggests that therapies targeting one pathway may not suffice, emphasizing the need for comprehensive genomic analysis to develop effective, personalized treatment plans.
Future Directions in FGFR3-Targeted Therapy
While FGFR3-targeted therapies show immense promise, more research is necessary to fully harness their potential. Key areas for future exploration include:
-
Combination Therapies:
Investigating the interplay between FGFR3 mutations and other genomic alterations like TP53 to create synergistic treatment strategies.
-
Access to Molecular Diagnostics:
Expanding the availability of molecular profiling in regions with high bladder cancer incidence, such as Asia, to ensure equitable access to precision medicine.
Considering advancements in targeted therapies, one of the major challenges remains targeted drug resistance, and there is an unmet crucial need to overcome the resistance. Hence, more research is warranted to understand appropriate synergistic partners tailored to the patient’s needs that can attenuate tumor growth locally without much interference in the patient’s overall well-being.
For an more details in context of Asian patients : Prevalence and Clinical Significance of FGFR3 Genomic Alterations in Asian Bladder Urothelial Carcinoma: A Systematic Review (Asian Journal of Oncology).
Interested in Advancing Precision Medicine?
Learn how genomic insights are transforming bladder cancer treatment. Get in touch to explore innovative oncology solutions.


